Medical term:
rheumatoid arthritis
Rheumatoid Arthritis
Definition
Description
Causes and symptoms
Diagnosis
Treatment
Alternative treatment
Prognosis
- race and gender (female and Caucasian).
- more than 20 joints involved.
- extremely high erythrocyte sedimentation rate.
- extremely high levels of rheumatoid factor.
- consistent, lasting inflammation.
- evidence of erosion of bone, joint, or cartilage on x rays.
- poverty.
- older age at diagnosis.
- rheumatoid nodules.
- other coexisting diseases.
- certain genetic characteristics, diagnosable through testing.
Prevention
Key terms
Resources
Books
Periodicals
arthritis
[ahr-thri´tis] (pl. arthri´tides)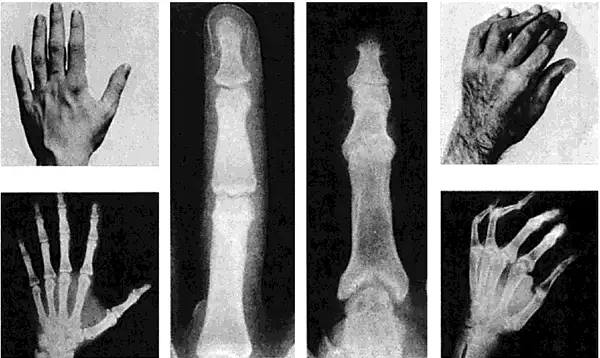
If untreated, and sometimes in spite of treatment, the joint pathology goes through four stages: (1) proliferative inflammation of the synovium with increased exudate, which eventually leads to thickening of the synovium; (2) formation of a layer of granulation tissue (pannus) that erodes and destroys the cartilage and eventually spreads to contiguous areas, causing destruction of the bone capsule and parts of the muscles that control the joint; (3) fibrous ankylosis resulting from invasion of the pannus by tough fibrous tissue; and (4) bony ankylosis as the fibrous tissue becomes calcified.
In addition to the joint changes there is atrophy of muscles, bones, and skin adjacent to the affected joint. The most characteristic lesions of rheumatoid arthritis are subcutaneous nodules, which may be present for weeks or months and are most commonly found over bony prominences, especially near the elbow.
Because rheumatoid arthritis is a systemic disease, there is involvement of connective tissues other than those in the musculoskeletal system. Degenerative lesions may be found in the collagen in the lungs, heart, blood vessels, and pleura.
Patients with rheumatoid arthritis appear undernourished and chronically ill. Most are anemic because of the effect of the disease on blood-forming organs. The erythrocyte sedimentation rate is elevated and the WBC may be slightly elevated.
The purpose of rest is to allow the body's natural defenses against inflammation to work at optimal level. It is necessary, however, even in the acute phase to balance rest with prescribed exercises which take into account the severity of the case, the joints affected, and the patient's individual needs and tolerance.
Therapeutic exercise is of major importance in the physical therapy program established for the patient. It is necessary to enlist the patient's cooperation, and this can be done most effectively by explaining the purposes of the exercises and teaching ways to exercise that will not increase pain. In many instances proper exercise can actually diminish pain. The patient's tolerance for exercise must be carefully monitored. While it is expected that some discomfort may be present during exercise, there should not be persistent pain that continues for hours after the exercises have been done. If such pain and fatigue do occur, the exercise program should be reviewed and revised so that a good balance of rest and exercise is obtained. It should be remembered that overactivity can contribute to the inflammatory process.
Applications of heat or cold may be used in the management of rheumatoid arthritis. Heat applications improve circulation, promote relaxation, and relieve pain. When used in conjunction with exercise, heat can allow more freedom of joint movement. Various forms of heat therapy may be used, including dry heat, moist heat, diathermy, and ultrasound. For dry heat a therapeutic infrared heat lamp may be most convenient during home care. Hot water bottles or electric heating pads also may be used. For treatment of the hands, paraffin baths are effective. Wet heat can be applied by hot tub baths with the water temperature not exceeding 39°C (102°F) or by means of a towel dipped in hot water, wrung out, and applied to the joint. Whirlpool baths are effective, especially when prolonged treatment is indicated. Relief from pain and stiffness can be provided for some patients by applications of cold packs to the affected joints. This can be done by placing ice packs directly over the joint. When either heat or cold is used, care must be taken to protect the patient's skin. It should be remembered that rheumatoid arthritis affects the skin as well as other tissues.
Whenever it is necessary to handle the joints and limbs of a patient with rheumatoid arthritis, it is extremely important to move slowly and gently, avoiding sudden, jarring movements which stimulate muscle contraction and produce pain. The affected joints should be supported so that there is no excessive motion.
Aspirin was among the first drugs used to treat rheumatoid arthritis and remains a low-cost treatment option. It is a potent antiinflammatory agent when given at dosages that achieve a serum level of 20–30 mg/100 ml. For those prone to stomach upset or other gastrointestinal side effects from aspirin, enteric-coated tablets or antacid mixtures of aspirin are available.
Other nonaspirin, nonsteroidal antiinflammatory drugs (NSAIDs) include the indole derivatives indomethacin, sulindac, and tolmetin and the phenylalkanoic acid derivatives fenoprofen, ibuprofen, and naproxen. Nowadays NSAIDs are the most used group of medications for treatment of arthritis. They may provide more relief than aspirin for certain patients, but they also may have side effects related to the gastrointestinal and nervous systems. COX-2 (cyclooxygenase-2) inhibitors are the latest class of NSAIDs. They have fewer gastrointestinal side effects than other NSAIDs.
Cytotoxic agents may also be used; these drugs act as immunosuppressants and block the inflammatory process of the disease. methotrexate is the most common of these. The dosage for the management of rheumatoid arthritis is much lower than the dosages for malignancies; thus the associated side effects are fewer. gold compounds or penicillamine may be prescribed for selected patients who cannot tolerate or are not responding well to more conservative methods of treatment.
The corticosteroids may be used in treating rheumatoid arthritis, but they are not a substitute for other forms of treatment. In some cases these drugs produce side effects that are more difficult to treat than arthritis. They also may worsen certain features of the disease rather than relieve them. Drugs included in this group are cortisone, hydrocortisone, prednisone, prednisolone, and dexamethasone.
Another group of medications that reduce inflammation are the biological response modifiers. Members of this group used to treat arthritis include etanercept and infliximab.
One surgical procedure employed is synovectomy (excision of the synovial membrane of a joint). The goal of this treatment is to interrupt the destructive inflammatory processes that eventually lead to ankylosis and invasion of surrounding cartilage and bone tissues.
Surgical repair of a hip joint (arthroplasty) may be performed when there is extensive damage and ambulation is not possible. The purpose of this procedure is to restore, improve, or maintain joint function. In cases in which it is not possible to restore the damaged hip joint there is a surgical procedure in which the diseased joint is completely replaced with a total hip prosthesis. The procedure is called a total hip replacement. A similar procedure involving total replacement of the knee can be done when there is extensive damage to the knee joint.
Braces, casts, or splints are sometimes used to immobilize the affected part so that it can rest during an active stage of the disease. Devices that immobilize the affected joint also may allow for motion of adjacent muscle, thereby improving muscle strength and permitting more independence on the part of the patient. Braces also may be used to prevent deformities by maintaining good position of the joints.
Home care is an essential part of the management of arthritis. To help in education of the public The Arthritis Foundation provides a number of pamphlets and other educational materials, supports a broad program of research and education, and helps finance improvement of local facilities for treatment of arthritis. The address of the foundation is The Arthritis Foundation, 1330 W. Peachtree St., Atlanta, GA 30309, telephone 404-872-7100.
rheu·ma·toid ar·thri·tis (RA),
[MIM*180300]rheumatoid arthritis
rheumatoid arthritis
Rheumatology A multisystem autoimmune disease characterized by chronic inflammation of multiple joints; RA is defined by the 1987 revised criteria, which requires that criteria 1-4 be present for > 6 wks Lab IgG autoantibodies, aka rheumatoid factors Management Etanercept ↓ disease activity in therapeutically refractive RArheu·ma·toid ar·thri·tis
(RA) (rū'mă-toyd ahr-thrī'tis)Synonym(s): arthritis deformans, nodose rheumatism (1) .


rheumatoid arthritis
Etiology
Factors implicated in the development and the severity of this disease include genetics (e.g., HLA haplotypes), autoimmune phenomena, and environmental influences.
Symptoms
Joint pains, morning stiffness, gelling, malaise, and fatigue are often present. Systemic disease marked by pleural effusions, pericarditis, pulmonary fibrosis, neuropathies, and ocular disorders may occu. Symptoms usually develop gradually over the course of several months but may begin abruptly in some patients.
Treatment
Most rheumatologists recommend aggressive therapy with disease-modifying antirheumatic drugs (DMARDs) early in the course of the illness to prevent bony erosions and loss of joint function. Drugs in this class include agents like methotrexate. Nonsteroidal anti-inflammatory drugs, e.g., ibuprofen or corticosteroids are often prescribed for palliation. Many patients may continue to take low-dose corticosteroids for years, but the benefits of long-term steroid use must be weighed against the risks, such as diabetes, osteoporosis, and adrenal suppression. Gold compounds can be used, but they are weaker than DMARDs and newer agents. Newer agents include antibodies to tumor necrosis factor and other immunomodulatory drugs. Powerful immunosuppressive agents like cyclosporine, azathioprine, and mycophenolate may also be used. Combination therapies involving several agents from different classes can be used. Joint replacement surgery can be helpful for some patients. Homeopathic substances such as black currant (gamma linolenic acid) and fish oil have demonstrated efficacy in rheumatoid arthritis
Patient care
All joints are assessed for inflammation, deformities, and contractures. The patient's ability to perform activities of daily living (ADLs) is evaluated. The patient is assessed for fatigue. Vital signs are monitored, and weight changes, pain (location, quality, severity, inciting and relieving factors), and morning stiffness (esp. duration) are documented. Use of moist heat is encouraged to relieve stiffness and pain. Prescribed anti-inflammatory and analgesic drugs are administered and evaluated; the patient is taught about the use of these medications. Patient response to all medications is evaluated, esp. after a change in drug regimen, and the patient and family are taught to recognize the purpose, schedule, and side effects of each. Over-the-counter drugs and herbal remedies may interact with prescribed drugs and should not be taken unless approved by physicians or pharmacists. Inflamed joints are occasionally splinted in extension to prevent contractures. Pressure areas are noted, and range of motion is maintained with gentle, passive exercise if the patient cannot comfortably perform active movement. Once inflammation has subsided, the patient is instructed in active range-of-motion exercise for specific joints. Warm baths or soaks are encouraged before or during exercise. Cleansing lotions or oils should be used for dry skin. The patient is encouraged to perform ADLs, if possible, allowing extra time as needed. Assistive and safety devices may be recommended for some patients. The patient should pace activities, alternate sitting and standing, and take short rest periods. Referral to an occupational or physical therapist helps keep joints in optimal condition as well as teaching the patient methods for simplifying activities and protecting joints. The importance of keeping PT/OT appointments and following home-care instructions should be stressed to both the patient and the family. A well-balanced diet that controls weight is recommended (obesity further stresses joints). Both patient and family should be referred to local and national support and information groups. Desired outcomes include cooperation with prescribed medication and exercise regimens, ability to perform ADLs, slowed progression of debilitating effects, pain control, and proper use of assistive devices. For more information and support, patient and family should contact the Arthritis Foundation (404-872-7100) (www.arthritis.org).
rheumatoid arthritis
A general disease affecting women more often than men and, in severe cases, causing progressive joint deformity, joint destruction and disability. The small joints of the fingers and hands are most seriously affected but the condition can spread to involve the wrists, elbows, shoulders and other joints. The disease is believed to be triggered by an infection that prompts the immune system to form damaging aggregates of ANTIGEN and ANTIBODY (IMMUNE COMPLEXES). The antibodies IgM, IgG and IgA (rheumatoid factors), and antibodies to COLLAGEN and cell nuclei, are present in the blood. Pro-inflammatory CYTOKINES, especially TUMOUR NECROSIS FACTOR are involved. Rheumatoid arthritis causes loss of appetite and weight, lethargy, muscle and tendon pain, nodules under the skin and often severe eye inflammation. There are many complications including ANAEMIA, PERICARDITIS, VASCULITIS and RAYNAUD'S PHENOMENON. Treatment is limited to control of inflammation and complications and the relief of pain by means of rest, splintage, physiotherapy and anti-inflammatory and painkilling drugs. Immunosuppressive drugs can be helpful and Penicillamine and gold are also widely used. See also STILL'S DISEASE (juvenile rheumatoid arthritis).arthritis, rheumatoid
rheu·ma·toid ar·thri·tis
(rū'mă-toyd ahr-thrī'tis) [MIM*180300]Synonym(s): arthritis deformans.
Patient discussion about rheumatoid arthritis
Q. Rheumatoid arthritis symptons?
there's also deformity of the hands (the fingers "deviates") and it can affect many systems in the body- lungs, liver, heart and blood vessels. so there can be many other symptoms.
Q. What Is the Cause for Rheumatoid Arthritis? I know rheumatoid arthritis is a disease that develops in adults. What causes this disease?
http://en.wikipedia.org/wiki/Image:Rheumatoid_arthritis_joint.gif
Q. Rheumatoid arthritis Is there any alternatives for my dearest friend who is suffering from Rheumatoid arthritis without having all prescribed drugs? I am fell sick when i see him struggling with more pain. Please help me to save him from pain.
here is more about the nutrition-arthritis connection:
http://ww2.arthritis.org/resources/nutrition/diet.asp
Latest Searches:
actinomycomata - acthib - acrospire - acrosin - acroscleroderma - acromiothoracic - acromioplasty - acrobystiolith - acrisorcin - AcQtrack - acorea - acoflex - acochoerus - acidogenic - acidity - acidimetries - acidimeter - achillotenotomy - achillodynia - acetylization -
- Service manuals - MBI Corp